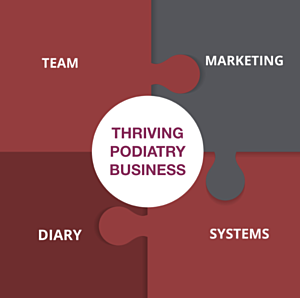
If you want to own and operate a Thriving Podiatry Business, there are four vital pieces to the business puzzle.
- Marketing - You need a well thought out marketing strategy, not just more tactics.
- Systems - You need systems that will support your marketing strategy and your team.
- Team - You need to develop a team culture that makes your work-life balance easier, not harder.
- Diary - Your diary needs to be structured in a way that maximises patient numbers and increases daily profits.
You have two choices: There's the slow approach, where you learn by trial and error and do everything yourself, or you can fast-track your education and business success with one-on-one business coaching and mentoring, or group coaching.
If you want to know more, please email me at and we can set up a Zoom Call and have a quick chat to see if I can be of assistance.
ALEX'S REFERENCES
THE ESSENTIAL PAIN PAPER
Moseley, G. L. (2007). Reconceptualising pain according to modern pain science. Physical Therapy Reviews, 12(3), 169-178. doi: 10.1179/108331907X223010
Pain papers:
Atlas, L. Y., & Wager, T. D. (2012). How expectations shape pain. Neuroscience Letters, 520(2), 140-148. doi: https://doi.org/10.1016/j.neulet.2012.03.039
Hainline, B., Turner, J. A., Caneiro, J. P., Stewart, M., & Lorimer Moseley, G. (2017). Pain in elite athletes—neurophysiological, biomechanical and psychosocial considerations: a narrative review. Br J Sports Med, 51(17), 1259-1264. doi: 10.1136/bjsports-2017-097890
Harvie, D. S., Broecker, M., Smith, R. T., Meulders, A., Madden, V. J., & Moseley, G. L. (2015). Bogus visual feedback alters onset of movement-evoked pain in people with neck pain. Psychol Sci, 26(4), 385-392. doi: 10.1177/0956797614563339
Rio, E., Moseley, L., Purdam, C., Samiric, T., Kidgell, D., Pearce, A. J., . . . Cook, J. (2014). The pain of tendinopathy: physiological or pathophysiological? Sports Med, 44(1), 9-23. doi: 10.1007/s40279-013-0096-z
Testa, M., & Rossettini, G. (2016). Enhance placebo, avoid nocebo: How contextual factors affect physiotherapy outcomes. Man Ther, 24, 65-74. doi: 10.1016/j.math.2016.04.006
Understanding complexity/complex systems theory:
Bittencourt, N. F. N., Meeuwisse, W. H., Mendonça, L. D., Nettel-Aguirre, A., Ocarino, J. M., & Fonseca, S. T. (2016). Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. Br J Sports Med, 50(21), 1309-1314. doi: 10.1136/bjsports-2015-095850
Stern, B. D., Hegedus, E. J., & Lai, Y. C. (2020). Injury prediction as a non-linear system. Phys Ther Sport, 41, 43-48. doi: 10.1016/j.ptsp.2019.10.010
Biopsychosocial model of health
Engel, G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science, 196(4286), 129-136. doi: 10.1126/science.847460
Engel, G. L. (1980). The clinical application of the biopsychosocial model. Am J Psychiatry, 137(5), 535-544. doi: 10.1176/ajp.137.5.535
Muscloskeletal Pain/Injury:
Caneiro, J. P., Roos, E. M., Barton, C. J., O'Sullivan, K., Kent, P., Lin, I., . . . O'Sullivan, P. (2020). It is time to move beyond ‘body region silos’ to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med, 54(8), 438-439. doi: 10.1136/bjsports-2018-100488
Lewis, J., & O’Sullivan, P. (2018). Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med, 52(24), 1543-1544. doi: 10.1136/bjsports-2018-099198
Lin, I., Wiles, L., Waller, R., Goucke, R., Nagree, Y., Gibberd, M., . . . O’Sullivan, P. P. B. (2020). What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med, 54(2), 79-86. doi: 10.1136/bjsports-2018-099878
Shared Decision Making:
Hoffmann, T. C., Lewis, J., & Maher, C. G. (2020). Shared decision making should be an integral part of physiotherapy practice. Physiotherapy, 107, 43-49. doi: https://doi.org/10.1016/j.physio.2019.08.012
Clinical Decision Making:
Simpkin, A. L., & Schwartzstein, R. M. (2016). Tolerating Uncertainty - The Next Medical Revolution? N Engl J Med, 375(18), 1713-1715. doi: 10.1056/NEJMp1606402
Walton, D. M. (2019). The critical skill of asking why? An endorsement of critical reflection in physiotherapy research and practice. Musculoskelet Sci Pract, 41, iv-v. doi: 10.1016/j.msksp.2019.04.005
Zou, K., Wong, J., Abdullah, N., Chen, X., Smith, T., Doherty, M., & Zhang, W. (2016). Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis, 75(11), 1964-1970. doi: 10.1136/annrheumdis-2015-208387
Communication:
Soklaridis, S., Hunter, J. J., & Ravitz, P. (2014). Twelve tips for asking and responding to difficult questions during a challenging clinical encounter. Med Teach, 36(9), 769-774. doi: 10.3109/0142159x.2014.916782
Zolnierek, K. B. H., & Dimatteo, M. R. (2009). Physician communication and patient adherence to treatment: a meta-analysis. Medical care, 47(8), 826-834. doi: 10.1097/MLR.0b013e31819a5acc